Physiotherapy For Bursitis Of The Foot
Bursitis is the inflammation of a bursa. Retrocalcaneal bursitis is in inflammation of the bursa located between the calcaneus and the anterior surface of the Achilles tendon.There are two bursae located just superior to the insertion of the Achilles (calcaneal) tendon. Anterior or deep to the tendon is the retrocalcaneal (subtendinous) bursa, which is located between the Achilles tendon and the calcaneus. Posterior or superficial to the Achilles tendon is the subcutaneous calcaneal bursa, also called the Achilles bursa. This bursa is located between the skin and posterior aspect of the distal Achilles tendon.Inflammation of either or both of these bursa can cause pain at the posterior heel and ankle region. It is also known as Achille tendon bursitis. It can often be mistaken for Achilles tendonitis or can also occur in conjunction with Achilles tendonitis.
Causes
Wearing poorly fitting or constrictive footwear can cause the heel to become irritated and inflamed. Shoes that dig into the back of the heel are the primary cause of retroachilles bursitis. Foot or ankle deformity. A foot or ankle deformity can make it more likely to develop retrocalcaneal bursitis. For example, some people can have an abnormal, prominent shape of the top of their heel, known as a Haglund's deformity. This condition increases the chances of irritating the bursa. A trauma to the affected heel, such as inadvertently striking the back of the heel against a hard object, can cause the bursa to fill with fluid, which in turn can irritate and inflame the bursa's synovial membrane. Even though the body usually reabsorbs the fluid, the membrane may stay inflamed, causing bursitis symptoms.
Symptoms
Symptoms of bursitis usually occur after rest and relaxation. Upon activity there is usually more intense pain in the area of the bursa. The common areas to have a bursitis in the foot are in the bottom of the heel, behind the heel near the attachment of the Achilles Tendon as well as along the side of a bunion. A bursa may also form in multiple areas especially along the metatarsal heads, or "ball" of your foot. You may actually feel the sac like fluid when rubbing the area of pain.
Diagnosis
Like all other forms of bursitis, initially the physician will take down the history of symptoms experienced by the patient, this will be followed by a detailed physical examination which involves checking for inflammation signs like pain, redness, and warmth of the heel area. The physician might examine further by moving the ankle a little to determine the exact location of pain. Further diagnostic tests including x-ray, bone scans, and MRI scan might be suggested if required.
Non Surgical Treatment
Conservative treatment of bursitis is usually effective. The application of heat, rest, and immobilization of the affected joint area is the first step. A sling can be used for a shoulder injury, a cane is helpful for hip problems. The patient can take nonsteroidal anti-inflammatory drugs (NSAIDs) like aspirin, ibuprofin, and naproxen. They can be obtained without a prescription and relieve the pain and inflammation. Once the pain decreases, exercises of the affected area can begin. If the nearby muscles have become weak because of the disease or prolonged immobility, then exercises to build strength and improve movement are best. A doctor or physical therapist can prescribe an effective regimen. If the bursitis is related to an inflammatory condition like arthritis or gout, then management of that disease is needed to control the bursitis. When bursitis does not respond to conservative treatment, an injection into the joint of a long-acting corticosteroid preparation, like prednisone, can bring immediate and lasting relief. A corticosteroid is a hormonal substance that is the most effective drug for reducing inflammation. The drug is mixed with a local anesthetic and works on the joint within five minutes. Usually one injection is all that is needed.
Surgical Treatment
Surgery to remove the damaged bursa may be performed in extreme cases. If the bursitis is caused by an infection, then additional treatment is needed. Septic bursitis is caused by the presence of a pus-forming organism, usually staphylococcus aureus. This is confirmed by examining a sample of the fluid in the bursa and requires treatment with antibiotics taken by mouth, injected into a muscle or into a vein (intravenously). The bursa will also need to be drained by needle two or three times over the first week of treatment. When a patient has such a serious infection, there may be underlying causes. There could be undiscovered diabetes, or an inefficient immune system caused by human immunodeficiency virus infection (HIV).
How To Fix Hammer Toes With Surgery
A Hammer toes can be flexible or rigid. Hammertoes often start out flexible and become rigid over time as your toe becomes accustomed to its crooked position. Flexible hammertoes are less serious than rigid hammertoes, as they can be easily diagnosed and treated in their initial stages. Flexible hammertoes are named as such because your affected toe still possesses some degree of movement.
Causes
Hammertoe is caused when muscles fail to work in a balanced manner and the toe joints bend to form the hammertoe shape. If they remain in this position, the muscles and tendons supporting them tighten and stay that way. Causes of hammertoe can include squeezing into a too-small or ill-fitting shoe or wearing high heels that jam your toes into a tight toe box. An injury such as badly stubbing your toe. Arthritis. Nerve and muscle damage from diseases such as diabetes,
 Symptoms
Symptoms
Some people never have troubles with hammer toes. In fact, some people don't even know they have them. They can become uncomfortable, especially while wearing shoes. Many people who develop symptoms with hammer toes will develop corns, blisters and pain on the top of the toe, where it rubs against the shoe or between the toes, where it rubs against the adjacent toe. You can also develop calluses on the balls of the feet, as well as cramping, aching and an overall fatigue in the foot and leg.
Diagnosis
Although hammertoes are readily apparent, to arrive at a diagnosis the foot and ankle surgeon will obtain a thorough history of your symptoms and examine your foot. During the physical examination, the doctor may attempt to reproduce your symptoms by manipulating your foot and will study the contractures of the toes. In addition, the foot and ankle surgeon may take x-rays to determine the degree of the deformities and assess any changes that may have occurred.
Non Surgical Treatment
Treatment options for a hammertoe are based on the severity of the condition. A hammertoe caused by inappropriate footwear can be corrected by wearing properly fitting shoes. If a high arch caused the condition, wearing toe pads or insoles in your shoes can help. These pads work by shifting your toe?s position, which relieves pain and corrects the appearance of your toe.
Surgical Treatment
Probably the most frequent procedure performed is one called a Post or an Arthroplasty. In this case a small piece of bone is removed from the joint to straighten the toe. The toe is shortened somewhat, but there is still motion within the toe post-operatively. In other cases, an Arthrodesis is performed. This involves fusing the abnormally-contracted joint. The Taylor procedure fuses only the first joint in the toe, whereas the Lambrinudi procedure fuses both joints within the toe. Toes which have had these procedures are usually perfectly straight, but they take longer to heal and don't bend afterwards. A Hibbs procedure is a transfer of the toe's long extensor tendon to the top of the metatarsal bone. The idea of this procedure is to remove the deforming cause of the hammertoes (in this case, extensor substitution), but to preserve the tendon's function in dorsifexing the foot by reattaching it to the metatarsals. Fortunately, the Gotch (or Gotch and Kreuz) procedure--the removal of the base of the toe where it attaches to the foot, is done less frequently than in years past. The problem with this procedure is that it doesn't address the problem at the level of the deformity, and it causes the toe to hammertoe become destabilized, often resulting in a toe that has contracted up and back onto the top of the foot. You can even have an Implant Arthroplasty procedure, where a small, false joint is inserted into place. There are several other procedures, as well.
 Prevention
Prevention
Be good to your feet, because they carry you. They are designed to last a lifetime, but that doesn?t mean they don?t need some love and care as well as some basic maintenance. Check your feet regularly for problems. This is especially true if you have diabetes or any other medical condition that causes poor circulation or numbness in your toes. If you do, check your feet every day so problems can be caught early on. Good circulation is essential. When you're sitting down, put your feet up. If you've been sitting for a while, stretch your legs and feet. Give yourself a foot massage, or ask someone you love for a foot massage. A warm foot bath is also a good idea.
Bunions Causes Signs Or Symptoms And Treatment
Overview
 A bunion (a.k.a Hallux Valgus) is a common foot condition associated with a prominent bump on the inside of the forefoot (see Figure 1). The word bunion? comes from the Greek root for the word turnip. Bunions can lead to discomfort over the prominence, especially if patients wear tight fitting shoes. It is common for bunions to run in family? and gradually increase over time. The vast majority of bunions can be managed successfully with basic non-operative treatment. Surgery is reserved for patients who have persistent symptoms in spite of appropriate non-operative treatment.
A bunion (a.k.a Hallux Valgus) is a common foot condition associated with a prominent bump on the inside of the forefoot (see Figure 1). The word bunion? comes from the Greek root for the word turnip. Bunions can lead to discomfort over the prominence, especially if patients wear tight fitting shoes. It is common for bunions to run in family? and gradually increase over time. The vast majority of bunions can be managed successfully with basic non-operative treatment. Surgery is reserved for patients who have persistent symptoms in spite of appropriate non-operative treatment.
Causes
Bunions are a common problem that can cause foot pain and difficulty wearing shoes. Bunions occur in about 30% of the population of most Western countries. They are seen most commonly in women and become more common as people get older. Patients with bunions generally have one of two problems that can cause pain. As the big toe becomes more and more angled (pointing toward the other toes), the base of the toe becomes more and more prominent, forming the bunion. The bunion forms in part because of the new angle of the toe, and in part due to inflammation over the bunion surface. As the inflammation worsens, people can experience pain with shoe wear and walking. The big toe may eventually come to lie over, or more commonly under, the second toe. This may cause further irritation while wearing shoes and more pain. The second toe of patients who have bunions commonly forms a hammer toe.
Symptoms
Bunions starts as the big toe begins to deviate, developing a firm bump on the inside edge of the foot, at the base of the big toe. Initially, at this stage the bunion may not be painful. Later as the toes deviate more the bunion can become painful, there may be redness, some swelling, or pain at or near the joint. The pain is most commonly due to two things, it can be from the pressure of the footwear on the bunion or it can be due to an arthritis like pain from the pressure inside the joint. The motion of the joint may be restricted or painful. A hammer toe of the second toe is common with bunions. Corns and calluses can develop on the bunion, the big toe and the second toe due to the alterations in pressure from the footwear. The pressure from the great toe on the other toes can also cause corns to develop on the outside of the little toe or between the toes. The change in pressure on the toe may predispose to an ingrown nail.
Diagnosis
Bunions are readily apparent - the prominence is visible at the base of the big toe or side of the foot. However, to fully evaluate the condition, the foot and ankle surgeon may take x-rays to determine the degree of the deformity and assess the changes that have occurred. Because bunions are progressive, they don?t go away, and will usually get worse over time. But not all cases are alike - some bunions progress more rapidly than others. Once your surgeon has evaluated your bunion, a treatment plan can be developed that is suited to your needs.
Non Surgical Treatment
Apply a commercial bunion pad around the bony prominence, use only non-medicated pads. Wear shoes with a wide and deep toe box. You should be able to "dimple" the leather over your bunion. Avoid all high heeled shoes. If your bunion becomes painful red, and swollen try elevating your foot and applying ice for about 20 minuets every hour. If symptoms persist, consult your podiatrist or physician. 
Surgical Treatment
The primary goal of bunion surgery is to relieve the pain associated with the deformity. This is accomplished by correcting the underlying abnormal metatarsal position by realigning it toward the second toe. Removing excessive bone formation on the bunion "bump", releasing the soft tissue tightness which is pulling the big toe towards the second toe. Tightening the soft tissues which are overly stretched on the bump side of the joint. Re-establish the correct alignment of the cartilage surfaces. Move the sesamoid bones into correct alignment. Realign the great toe. Bunion surgery procedures are based on many factors, including health, age and lifestyle of the patient. However, a critical factor in procedure choice is the grading of the bunion deformity.
Overpronation Of The Feet
One of the most common causes of foot and leg discomfort is a condition known as over pronation. Normal pronation, or "turning inward", of the foot is necessary as the foot adapts to the ground. With over pronation, however, the arch flattens, collapses, and soft tissues stretch. This causes the joint surfaces to function at unnatural angles to each other. When this happens, joints that should be stable now become very loose and flexible. At first, over pronation may cause fatigue. As the problem gets worse, strain on the muscles, tendons, and ligaments of the foot and lower leg can cause permanent problems and deformities.

Causes
Over-pronation may happen because the tissue that attaches to your foot bones is loose. You may be born with this problem or it may result from injuries or overuse, like from too much running.
Symptoms
Overpronation can negatively affect overall body alignment. The lowering of the longitudinal arch pulls the heel bone in, causing the leg, thigh bone and hip to rotate inwards, and an anterior tilt of the pelvis. Unnecessary strain to the ankles, knees, hips and back can result. Plantar fasciitis and inflammation, metatarsal pain, problems with the Achilles tendon, pain on the inside of the knee, and bursitis in the hip are just some of the conditions commonly associated with pronation.
Diagnosis
When you overpronate your foot rolls inwards causing the lower leg to rotate inwards too. It's thought that this increases stress on the soft tissues of the lower leg causing pain and inflammation, or more commonly known as shin splints.

Non Surgical Treatment
Solutions typically presented will include physical therapy sessions, prolonged prescription drug regimens, occasionally non-traditional approaches like holistic medicine and acupuncture. These options can provide symptom relief in the short term for some patients. However, these treatment methods cannot correct the internal osseous misalignment. Ligaments are not effective in limiting the motion of the ankle bone when excessive joint motion is present. Furthermore, there is not a single, specific ligament that is "too tight" that needs to be "stretched out." The muscles supporting the bones are already being "over-worked" and they cannot be strengthened enough to realign these bones. There is no evidence to suggest that any of these measures are effective in re-establishing or maintaining the normal joint alignment and function.
Prevention
With every step we take, we place at least half of our body weight on each foot (as we walk faster, or run, we can exert more than twice our body weight on each foot). As this amount of weight is applied to each foot there is a significant shock passed on to our body. Custom-made orthotics will absorb some of this shock, helping to protect our feet, ankles, knees, hips, and lower back.
What Exactly Is Calcaneal Apophysitis?
Sever's disease is a pain that occurs in the back of the heel of physically active children at around the time of puberty. Sever's disease occurs due to an inflammation of the growth plate due to excessive pull of the achilles tendon on this growth plate. During puberty the bones quite often grow faster than the muscles and tendons causing the tendons to become tight, this tightness then results in excessive pull on the back of the heel resulting in this painful condition.
Causes
Sever disease is more common in children who do regular sports or exercise that puts pressure on the heels. Activities such as running and jumping can put stress on the tight muscles and tendons.
Symptoms
The most prominent symptom of Sever?s disease is heel pain which is usually aggravated by physical activity such as walking, running or jumping. The pain is localised to the posterior and plantar side of the heel over the calcaneal apophysis. Sometimes, the pain may be so severe that it may cause limping and interfere with physical performance in sports. External appearance of the heel is almost always normal, and signs of local disease such as edema, erythema (redness) are absent. The main diagnostic tool is pain on medial- lateral compression of the calcaneus in the area of growth plate, so called squeeze test. Foot radiographs are usually normal. Therefore the diagnosis of Sever?s disease is primarily clinical.
Diagnosis
Sever?s disease can be diagnosed based on the symptoms your child has. Your child?s doctor will conduct a physical examination by squeezing different parts of your child?s foot to see if they cause any pain. An X-ray may be used to rule out other problems, such as a broken bone or fracture.
Non Surgical Treatment
The initial treatment is rest, relieve the pain and treat the underlying cause. The foot and ankle should be rested so that the apophysis it is not being continually ?injured?. A small heel (sorbothane heel insert) raise can used to raise the heel and take the stretch off the Achilles tendon. It may be sufficient to stop your child playing sport but some children require a short period of bed or couch rest. Some children find resting very difficult and require the use of braces or plasters or boots to slow them down. Using crutches is advised. Severs is usually caused by tight muscles. A stretching program should be followed usually supervised by a physiotherapist. The stretching program may need to be undertaken up to 5 times a day. If flat feet are a problems orthotics (insoles) should be used. The pain should be controlled by rest (limiting activity) and ice (icing the painful area 3-4 times a day - making sure the skin is not burnt), Simple pain killers can be used such as paracetamol as well as anti-inflammatory tablets and cream. Severs disease usually goes away with time. When your child stops growing, the pain and swelling should go away because the growing (weak) area fuses and becomes solid bone which is very strong.
Prevention
To prevent Sever's Disease, fit your child with kid's shoes with good cushioning in the footbed, shock absorption in the heel, and support in the outsole. Make sure children wear supportive shoes, especially when they're running and jumping, to reduce the impact on the heel and strain on the developing bone and muscle structure of a kids' feet. Children's arch supports and heel cups comfortably support the foot and encourage healthy alignment while your child runs or walks.
What Are The Causes Of Achilles Tendon Rupture
Overview
 The Achilles tendon is the confluence of the independent tendons of the gastrocnemius and soleus, which fuse to become the Achilles tendon approximately 5 to 6 cm proximal to its insertion on the posterior surface of the calcaneus. The gastrocnemius and soleus muscles, via the Achilles tendon, function as the chief plantarflexors of the ankle joint. This musculotendinous unit provides the primary propulsive force for walking, running, and jumping. The normal Achilles tendon can withstand repetitive loads near its ultimate tensile strength, which approach 6 to 8 times body weight.
The Achilles tendon is the confluence of the independent tendons of the gastrocnemius and soleus, which fuse to become the Achilles tendon approximately 5 to 6 cm proximal to its insertion on the posterior surface of the calcaneus. The gastrocnemius and soleus muscles, via the Achilles tendon, function as the chief plantarflexors of the ankle joint. This musculotendinous unit provides the primary propulsive force for walking, running, and jumping. The normal Achilles tendon can withstand repetitive loads near its ultimate tensile strength, which approach 6 to 8 times body weight.
Causes
The Achilles tendon is most commonly injured by sudden plantarflexion or dorsiflexion of the ankle, or by forced dorsiflexion of the ankle outside its normal range of motion. Other mechanisms by which the Achilles can be torn involve sudden direct trauma to the tendon, or sudden activation of the Achilles after atrophy from prolonged periods of inactivity. Some other common tears can occur from overuse while participating in intense sports. Twisting or jerking motions can also contribute to injury. Fluoroquinolone antibiotics, famously ciprofloxacin, are known to increase the risk of tendon rupture, particularly achilles.
Symptoms
Although it's possible to have no signs or symptoms with an Achilles tendon rupture, most people experience pain, possibly severe, and swelling near your heel, an inability to bend your foot downward or "push off" the injured leg when you walk, an inability to stand on your toes on the injured leg, a popping or snapping sound when the injury occurs. Seek medical advice immediately if you feel a pop or snap in your heel, especially if you can't walk properly afterward.
Diagnosis
The diagnosis of an Achilles tendon rupture can be made easily by an orthopedic surgeon. The defect in the tendon is easy to see and to palpate. No x-ray, MRI or other tests are necessary.
Non Surgical Treatment
Not every torn Achilles tendon needs an operation. Recent studies have shown that even a conservative treatment, i.e. immobilizingt the leg can lead to satisfactory healing successes. This requires, however, that the patient is fitted with a cast (immobilization splint) and/or a special boot for a period of approximately 6 - 8 weeks. After that, the boot must be worn during the day for about two more weeks. An intensive physiotherapy will start after about six weeks to train the calf muscles so that the initial coordination can be restored. Running training on flat ground can be started again after another 10 - 12 weeks. Studies show that the danger of a recurring torn tendon is higher after a conservative treatment opposed to an operative treatment. Depending on the type of treatment, about 10 - 15 percent of those affected can expect at some point to again suffer from a tear of the Achilles tendon. Moreover, in the non-operated cases, we see more often a significant permanent weakness of the footprint, particularly restricting the ability to participate in sports. 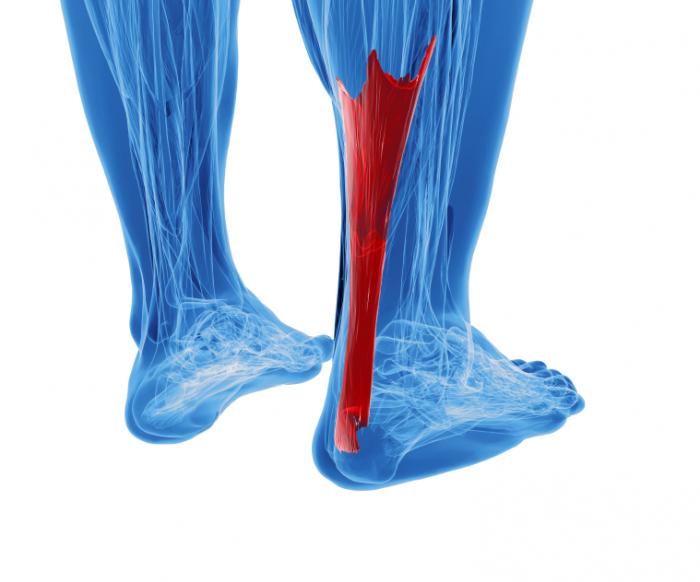
Surgical Treatment
Surgery may be indicated directly following injury rather than conservative care. Repair of an achilles tendon rupture is greatly varied for each clinical situation. There may be a direct repair of the ends of the tendon with suture, or possibly a tendon graft used to augment the tendon. Post-operatively, the period of immobilization will depend on the size of the defect that was repaired and how it was completed. Usually the immobilization is between 6-10 weeks. This repair may allow for a complete return to normal function, but in many instances the healing is complicated with adhesions and a partial loss of range of motion. There may be a continued soft tissue defect noted and a permanent or prolonged swelling.
Prevention
The following can significantly reduce the risk of Achilles tendon rupture. Adequate stretching and warming up prior to exercising. If playing a seasonal sport, undertake preparatory exercises to build strength and endurance before the sporting season commences. Maintain a healthy body weight. This will reduce the load on the tendon and muscles. Use footwear appropriate for the sport or exercise being undertaken. Exercise within fitness limits and follow a sensible exercise programme. Increase exercise gradually and avoid unfamiliar strenuous exercise. Gradual ?warm down? after exercising.
The Treatment And Cause
Overview
Adult Acquired Flatfoot (Posterior Tibial Tendon Dysfunction) is a painful, progressive deformity in adults. It results from a gradual stretch (attenuation) of the tibialis posterior tendon and the ligaments that support your foot?s arch. This stretching causes the tendon to lose strength and function. Many people have flat feet and do not experience pain. However, pain occurs with Adult Acquired Flatfoot because the tendons and ligaments have been torn. Once the vital ligaments and posterior tibial tendon are lost, there is no longer anything holding the arch of the foot in place. 
Causes
There are a number of theories as to why the tendon becomes inflamed and stops working. It may be related to the poor blood supply within the tendon. Increasing age, inflammatory arthritis, diabetes and obesity have been found to be causes.
Symptoms
Patients will usually describe their initial symptoms as "ankle pain", as the PT Tendon becomes painful around the inside of the ankle joint. The pain will become more intense as the foot flattens out, due to the continued stretching and tearing of the PT Tendon. As the arches continue to fall, and pronation increases, the heel bone (Calcaneus) tilts into a position where it pinches against the ankle bone (Fibula), causing pain on both the inside and outside of the ankle. As the foot spends increased time in a flattened, or deformed position, Arthritis can begin to affect the joints of the foot, causing additional pain.
Diagnosis
Posterior Tibial Tendon Dysfunction is diagnosed with careful clinical observation of the patient?s gait (walking), range of motion testing for the foot and ankle joints, and diagnostic imaging. People with flatfoot deformity walk with the heel angled outward, also called over-pronation. Although it is normal for the arch to impact the ground for shock absorption, people with PTTD have an arch that fully collapses to the ground and does not reform an arch during the entire gait period. After evaluating the ambulation pattern, the foot and ankle range of motion should be tested. Usually the affected foot will have decreased motion to the ankle joint and the hindfoot. Muscle strength may also be weaker as well. An easy test to perform for PTTD is the single heel raise where the patient is asked to raise up on the ball of his or her effected foot. A normal foot type can lift up on the toes without pain and the heel will invert slightly once the person has fully raised the heel up during the test. In early phases of PTTD the patient may be able to lift up the heel but the heel will not invert. An elongated or torn posterior tibial tendon, which is a mid to late finding of PTTD, will prohibit the patient from fully rising up on the heel and will cause intense pain to the arch. Finally diagnostic imaging, although used alone cannot diagnose PTTD, can provide additional information for an accurate diagnosis of flatfoot deformity. Xrays of the foot can show the practitioner important angular relationships of the hindfoot and forefoot which help diagnose flatfoot deformity. Most of the time, an MRI is not needed to diagnose PTTD but is a tool that should be considered in advanced cases of flatfoot deformity. If a partial tear of the posterior tibial tendon is of concern, then an MRI can show the anatomic location of the tear and the extensiveness of the injury.
Non surgical Treatment
PTTD is a progressive condition. Early treatment is needed to prevent relentless progression to a more advanced disease which can lead to more problems for that affected foot. In general, the treatments include rest. Reducing or even stopping activities that worsen the pain is the initial step. Switching to low-impact exercise such as cycling, elliptical trainers, or swimming is helpful. These activities do not put a large impact load on the foot. Ice. Apply cold packs on the most painful area of the posterior tibial tendon frequently to keep down the swelling. Placing ice over the tendon immediately after completing an exercise helps to decrease the inflammation around the tendon. Nonsteroidal Anti-inflammatory Medication (NSAIDS). Drugs, such as arcoxia, voltaren and celebrex help to reduce pain and inflammation. Taking such medications prior to an exercise activity helps to limit inflammation around the tendon. However, long term use of these drugs can be harmful to you with side effects including peptic ulcer disease and renal impairment or failure. Casting. A short leg cast or walking boot may be used for 6 to 8 weeks in the acutely painful foot. This allows the tendon to rest and the swelling to go down. However, a cast causes the other muscles of the leg to atrophy (decrease in strength) and thus is only used if no other conservative treatment works. Most people can be helped with orthotics and braces. An orthotic is a shoe insert. It is the most common non-surgical treatment for a flatfoot and it is very safe to use. A custom orthotic is required in patients who have moderate to severe changes in the shape of the foot. Physiotherapy helps to strengthen the injured tendon and it can help patients with mild to moderate disease of the posterior tibial tendon. 
Surgical Treatment
Many operations are available for the treatment of dysfunction of the posterior tibial tendon after a thorough program of non-operative treatment has failed. The type of operation that is selected is determined by the age, weight, and level of activity of the patient as well as the extent of the deformity. The clinical stages outlined previously are a useful guide to operative care (Table I). In general, the clinician should perform the least invasive procedure that will decrease pain and improve function. One should consider the effects of each procedure, particularly those of arthrodesis, on the function of the rest of the foot and ankle.